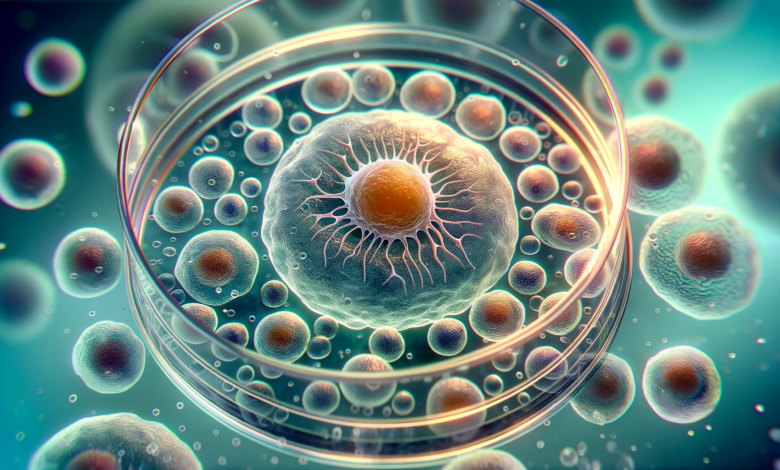
Stem cells are present in various organs and tissues throughout the human body. Each type of stem cell is typically associated with specific organs and has different capacities for differentiation and regeneration. Some of the key organs and tissues where stem cells are found include:
1- Stem Cells in Bone Marrow
This is one of the most well-known sources of adult stem cells. Bone marrow stem cells can differentiate into a variety of cell types, including those that make up the blood and immune system (like red blood cells, white blood cells, and platelets).
- Hematopoietic Stem Cells (HSCs): These are perhaps the most well-known and extensively studied type of stem cells found in bone marrow. HSCs are responsible for the production of all the blood cells in the body. This process, known as hematopoiesis, involves the differentiation of HSCs into various types of blood cells, including:
- Red Blood Cells (Erythrocytes): Responsible for carrying oxygen to tissues.
- White Blood Cells (Leukocytes): Key players in the immune system, with different types of white blood cells having various roles in defending the body against infection and disease.
- Platelets (Thrombocytes): Essential for blood clotting and wound healing.
- Mesenchymal Stem Cells (MSCs): These cells are also found in bone marrow (though they can be found in other tissues as well, such as fat tissue). MSCs can differentiate into various types of cells including:
- Osteoblasts: Cells that form bone.
- Chondrocytes: Cells that form cartilage.
- Adipocytes: Cells that form fat tissue.
- Myocytes: Cells that can form muscle.
Bone marrow stem cells, particularly HSCs, have been used for decades in bone marrow transplants, which can be life-saving treatments for patients with conditions like leukemia, lymphoma, and other blood disorders. The process involves transplanting healthy HSCs into a patient, where they can generate new, healthy blood cells, effectively replacing the cells affected by disease.
MSCs from bone marrow are being researched for their potential in regenerative medicine, given their ability to differentiate into a variety of cell types. They are being studied for use in repairing damaged tissues, treating autoimmune diseases, and in various other therapeutic applications.
2- Stem cells in Brain
Neural stem cells in the brain can give rise to its main constituents: neurons, astrocytes, and oligodendrocytes.
Brain stem cells are a specialized group of cells within the central nervous system that have the potential to differentiate into various types of neural cells. These stem cells are crucial for brain development, maintenance, and repair. There are two primary types of stem cells in the brain:
Neural Stem Cells (NSCs): These are multipotent stem cells capable of differentiating into the three major cell types of the central nervous system:
- Neurons: The primary functional cells of the brain and nervous system, responsible for transmitting and processing information through electrical and chemical signals.
- Astrocytes: Glial cells that provide support and nutrition to neurons, maintain the blood-brain barrier, and perform various other critical functions in the central nervous system.
- Oligodendrocytes: Another type of glial cell, responsible for creating myelin sheaths around the axons of neurons, which helps in the rapid transmission of electrical signals.
Neural Progenitor Cells (NPCs): These are a more restricted type of stem cell found in the brain. They are typically already committed to a specific neural lineage, meaning they will differentiate into a specific type of neural cell.
Brain stem cells are primarily located in two areas:
- Subventricular Zone (SVZ): This is a layer of tissue in the walls of the lateral ventricles in the brain, where NSCs can give rise to new neurons and glial cells.
- Hippocampus (specifically the Dentate Gyrus): This region is involved in memory and learning, and it’s one of the few areas in the brain where neurogenesis (the creation of new neurons) is known to occur throughout life.
During embryonic development and early postnatal life, brain stem cells are heavily involved in the formation of the brain’s structure and the establishment of neural networks. In adults, brain stem cells contribute to the maintenance of neural circuits and have some capacity for repair following injury. However, this regenerative ability is quite limited compared to other tissues like skin or blood.
There’s significant interest in using brain stem cells for regenerative therapies to treat conditions like Parkinson’s disease, Alzheimer’s disease, spinal cord injuries, and stroke. The idea is to replace damaged or lost neurons and restore brain function. Brain stem cells, particularly those derived from induced pluripotent stem cells (iPSCs), are used to create models of human neurological diseases, which are invaluable for drug testing and understanding disease mechanisms.
The use of brain stem cells in therapy and research is a rapidly advancing field but comes with substantial challenges. The complexity of the brain, the difficulty in accessing these cells, and the limited capacity of neurons to regenerate are significant hurdles. Furthermore, ensuring the integration and proper functioning of new neurons within existing neural networks is a complex task that researchers are still working to understand and achieve.
3- Stem Cells and Skin
The skin contains stem cells in the basal layer of the epidermis and in the hair follicles. These cells are key for skin regeneration and repair.
Skin stem cells are a vital component of the skin’s regenerative capabilities, playing a key role in the maintenance, repair, and renewal of the skin. The skin is the largest organ of the body and consists of two main layers: the epidermis (outer layer) and the dermis (underlying layer). Each layer hosts different types of stem cells:
- Epidermal Stem Cells: These are found in the basal layer of the epidermis. They are responsible for generating new skin cells (keratinocytes), which then migrate upwards to form the outer protective layer of the skin. These cells continuously divide to replace the skin cells that are constantly being shed.
- Hair Follicle Stem Cells: Located in the hair follicle bulge region, these stem cells contribute to the growth of hair. They can also participate in the repair of the epidermis after injury.
- Melanocyte Stem Cells: Found in the hair follicles and the basal layer of the epidermis, these cells produce melanocytes, which are responsible for the pigmentation of the skin and hair.
- Sebaceous Gland Stem Cells: These cells are responsible for replenishing the cells in the sebaceous glands, which produce the skin’s natural oils.
- Mesenchymal Stem Cells in the Dermis: These cells can differentiate into various cell types, including fibroblasts, which produce collagen and other extracellular matrix components essential for skin structure and elasticity.
Skin Renewal: The skin undergoes continuous renewal throughout life, and skin stem cells are crucial for this process. They ensure that the skin maintains its integrity and barrier function.
Wound Healing: In response to skin injury, stem cells are activated to repair damaged tissues, promoting wound closure and re-epithelialization.
Hair Growth: Hair follicle stem cells are periodically activated to induce new hair growth cycles.
In the realm of medical research and therapeutic applications, skin stem cells have emerged as a cornerstone, particularly in regenerative medicine, disease treatment, and cosmetic and anti-aging research. In regenerative medicine, these cells are pivotal for treating burns, ulcers, and other skin injuries, with laboratory-grown skin grafts from stem cells already proving successful in treating severe burn victims. The scope of research extends into disease treatment, focusing on a deeper understanding and effective management of various skin diseases, including the challenges posed by skin cancers, genetic skin disorders, and aging-related skin changes. Moreover, the role of skin stem cells in the aging process is a rapidly growing area of interest, particularly in developing potential anti-aging treatments. This research aims to harness the regenerative capabilities of these cells to offer innovative solutions for age-related skin issues, marking a significant stride in both healthcare and cosmetic fields.
Despite the considerable potential, there are challenges in skin stem cell research and therapy, such as ensuring the long-term survival and integration of transplanted cells and avoiding the risk of tumor formation. Additionally, understanding the complex signaling pathways that regulate skin stem cell behavior is crucial for effectively harnessing their therapeutic potential.
4- Liver Stem Cells
Liver stem cells, also known as hepatic stem cells, are a type of stem cell found in the liver. They are of great interest in medical research due to their potential in regenerative medicine and liver disease treatment. Here are some key points about liver stem cells:
Regeneration and Repair: The liver is known for its remarkable ability to regenerate. Liver stem cells play a crucial role in this process. They have the potential to differentiate into various cell types within the liver, aiding in tissue repair and regeneration.
Treatment of Liver Diseases: Liver stem cells are being studied for their potential to treat a range of liver diseases, including cirrhosis, hepatitis, and liver cancer. By replacing damaged or diseased cells, they offer a promising avenue for therapies that could restore liver function in patients with severe liver conditions.
Liver Transplantation: In the context of liver transplantation, liver stem cells might provide an alternative to whole organ transplants. Research is focused on using these cells to grow liver tissue in the lab, which could be transplanted into patients, potentially reducing the need for donor organs.
Modeling Liver Diseases: Liver stem cells are also useful in the laboratory for modeling liver diseases. Scientists can study these cells to understand the progression of liver diseases better and to test new drugs and treatments in a controlled environment.
The field of liver stem cell research is rapidly evolving, offering exciting possibilities for advancing our understanding and treatment of liver diseases.
5- Muscle Stem Cells
Muscle stem cells, often referred to as satellite cells, play a crucial role in the growth, repair, and regeneration of skeletal muscles. They are a specialized type of stem cell that resides within muscle tissues. Here are some key aspects of muscle stem cells:
Repair and Regeneration: Muscle stem cells are primarily responsible for repairing and regenerating muscle fibers after injury or damage. When muscle damage occurs, these cells are activated, proliferate, and differentiate into mature muscle fibers, aiding in the repair process.
Muscle Growth: In response to exercise or muscle growth requirements, muscle stem cells contribute to the increase in muscle mass. They are essential for hypertrophic growth, where muscle fibers increase in size.
Aging and Muscle Degeneration: As we age, the number and functionality of muscle stem cells decline, leading to a reduced capacity for muscle regeneration. This decline is a significant factor in age-related muscle loss, known as sarcopenia.
Duchenne Muscular Dystrophy (DMD) and Other Disorders: Research on muscle stem cells has implications for understanding and treating muscular dystrophies, such as Duchenne Muscular Dystrophy (DMD). By studying how these cells function and regenerate muscle tissue, scientists hope to develop therapies to treat or alleviate symptoms of these conditions.
Overall, muscle stem cells are a vital area of study with significant implications for treating muscle-related injuries and conditions, and their role in muscle health and disease continues to be a subject of intense research and interest.
6- Intestinal Stem Cells
Stem cells in the intestinal mucosa are a vital component in the maintenance, repair, and regeneration of the intestinal lining. The intestinal mucosa is a rapidly self-renewing tissue in the body, and its stem cells play a critical role in this process. Here are some key points about these stem cells:
Location and Function: Intestinal stem cells are primarily located at the base of the crypts of Lieberkühn in the epithelium of the small intestine and colon. They are responsible for continuously generating all cell types of the intestinal epithelium, including absorptive enterocytes, goblet cells, enteroendocrine cells, and Paneth cells.
Rapid Turnover: The intestinal epithelium is one of the fastest-renewing tissues in the human body. This rapid turnover is driven by the intestinal stem cells, which divide regularly to produce new cells that replace the older cells shed from the villus tips.
Regeneration and Healing: After injury or damage, such as that caused by inflammation, infection, or certain medical treatments like chemotherapy, these stem cells are crucial for repairing and regenerating the intestinal lining.
Cancer Research: Intestinal stem cells are a focus of cancer research, particularly in understanding how mutations in these cells can lead to colorectal cancer. Understanding the behavior of these stem cells in normal and disease states is essential for developing targeted therapies.
Gut Microbiome Interaction: Recent studies suggest that intestinal stem cells interact with the gut microbiome. The microbiota can influence stem cell function and, consequently, the overall health and disease state of the intestine.
Therapeutic Potential: There is growing interest in harnessing intestinal stem cells for treating various gastrointestinal disorders, such as inflammatory bowel disease (IBD), Crohn’s disease, ulcerative colitis, and short bowel syndrome. Research is ongoing to explore the potential of these cells in regenerative medicine.
Overall, stem cells in the intestinal mucosa are a key area of study due to their fundamental role in maintaining intestinal health, their potential in regenerative medicine, and their involvement in various gastrointestinal diseases.
7- Stem Cells in Adipose Tissue
Adipose tissue stem cells, often referred to as adipose-derived stem cells (ASCs), are a type of mesenchymal stem cell found in fat tissue. They have gained significant attention in both research and clinical applications due to their abundance, ease of harvest, and potential in regenerative medicine. Here are some key aspects of adipose tissue stem cells:
Source and Harvesting: Adipose tissue stem cells are derived from fat tissue, which can be easily obtained through liposuction procedures. This makes them more accessible and less invasive to harvest compared to other types of stem cells, such as those from bone marrow.
Differentiation Potential: Similar to other mesenchymal stem cells, ASCs have the ability to differentiate into various cell types, including osteoblasts (bone cells), chondrocytes (cartilage cells), myocytes (muscle cells), and adipocytes (fat cells). This multipotency makes them a valuable resource for regenerative therapies.
Regenerative Medicine Applications: ASCs are being explored for their use in a variety of regenerative medicine applications, such as in the healing of wounds, treatment of chronic ulcers, and reconstruction of soft tissues damaged by injury or surgery. Their ability to promote tissue repair and modulate immune responses is particularly valuable.
Tissue Engineering: In tissue engineering, adipose tissue stem cells are used to create bioengineered tissues that can replace damaged or diseased tissues in the body. They are often combined with scaffolds and growth factors to facilitate tissue regeneration.
Research in Autoimmune Diseases and Inflammation: Due to their immunomodulatory properties, ASCs are a subject of study in the treatment of autoimmune diseases and inflammatory conditions. They have the potential to modulate the immune system’s response and reduce inflammation.
Cosmetic and Plastic Surgery: In the field of cosmetic and plastic surgery, ASCs are being used for soft tissue augmentation, including facial rejuvenation and breast reconstruction. Their ability to differentiate into adipocytes is particularly useful in these applications.
Adipose tissue stem cells offer a promising and versatile tool in the field of regenerative medicine, and their relatively easy and minimally invasive extraction process makes them a highly attractive source of stem cells for various therapeutic applications.
8- Heart Stem Cells
Heart stem cells, also known as cardiac stem cells, are a type of stem cell found within the heart. They have garnered significant interest in the field of regenerative medicine, particularly for their potential in repairing and regenerating heart tissue, which is especially relevant in the context of heart disease and heart failure. Here are some key aspects of heart stem cells:
Regeneration of Heart Tissue: Unlike most other cells in the heart, cardiac stem cells have the potential to divide and differentiate into various types of heart cells. This ability is crucial for the repair and regeneration of damaged heart tissue, which is particularly important after events like heart attacks.
Treatment of Heart Diseases: Heart stem cells are being studied for their potential in treating various heart conditions, including myocardial infarction (heart attack), cardiomyopathy, and heart failure. By regenerating damaged heart tissue, these cells could improve heart function and outcomes for patients with heart diseases.
Challenges in Adult Hearts: One of the challenges in utilizing heart stem cells is that the adult heart has a limited number of these cells and a low capacity for self-repair. Research is focused on finding ways to activate or augment these cells to enhance heart repair.
Stem Cell Transplantation and Therapy: Scientists are exploring methods such as transplanting heart stem cells or stem cells from other sources (like bone marrow) into the heart. The aim is to encourage the repair and regeneration of heart tissue, either by direct differentiation of these cells into heart tissue or by the cells releasing factors that aid in healing.
Potential in Tissue Engineering: There’s also interest in using heart stem cells in tissue engineering, potentially growing heart tissue in the lab for transplantation, which could offer new treatment avenues for heart disease patients.
Heart stem cells represent an exciting area of research with the potential to revolutionize the treatment of heart diseases. However, there’s still much to learn about these cells, their capabilities, and the best ways to harness them for therapeutic purposes.
9- Dental Stem Cells
Dental stem cells are a unique type of stem cell found within the oral cavity, specifically in dental tissues such as the dental pulp, periodontal ligament, and tooth germ. These cells have generated significant interest in the field of regenerative dentistry and medicine due to their potential in repairing and regenerating dental and other bodily tissues. Here are some key points about dental stem cells:
Types and Locations: Several types of dental stem cells have been identified, including dental pulp stem cells (DPSCs), stem cells from human exfoliated deciduous teeth (SHED), periodontal ligament stem cells (PDLSCs), stem cells from apical papilla (SCAP), and dental follicle progenitor cells (DFPCs). Each type is located in different parts of the tooth and surrounding structures.
Dental Tissue Regeneration: Dental stem cells can differentiate into various cell types, making them valuable for regenerating dental tissues. They have the potential to regenerate dentin, pulp, periodontal ligament, and even alveolar bone. This capability is significant for developing treatments for dental diseases and injuries, such as tooth decay and periodontal disease.
Potential Beyond Dentistry: Research suggests that dental stem cells could have applications beyond regenerative dentistry. They might be used to regenerate non-dental tissues, such as neural cells, bone, and cartilage. This broad potential makes them an exciting area of study in regenerative medicine.
Tooth Repair and Replacement: Dental stem cells offer prospects for bioengineering teeth as a replacement for lost or damaged ones. Research in this area aims to develop ways to grow whole teeth in vitro to be transplanted as functional replacements for lost teeth.
Cryopreservation and Banking: The fact that dental stem cells can be harvested from deciduous (baby) teeth or wisdom teeth extractions makes them accessible. There’s growing interest in the cryopreservation and banking of dental stem cells for future therapeutic use, similar to cord blood banking.
Dental stem cells represent a promising frontier in regenerative medicine and dentistry, offering potential innovations in the treatment of a wide range of dental and other health conditions. Their ability to regenerate tissues and the relative ease of their procurement make them a significant focus of current research.
10- Cornea Stem Cells
Cornea stem cells, primarily known as limbal stem cells, are a specialized type of stem cell located in the limbus, the border area between the cornea and the conjunctiva of the eye. These cells play a crucial role in maintaining and repairing the corneal epithelium, the outermost layer of the cornea. Here are some key aspects of cornea stem cells:
Role in Corneal Health: Limbal stem cells are essential for the continuous regeneration of the corneal epithelium. They help maintain the transparency and integrity of the cornea, which is crucial for vision.
Treatment of Corneal Diseases: Damage or loss of limbal stem cells can lead to limbal stem cell deficiency (LSCD), a condition that results in the loss of corneal clarity and vision impairment. Transplantation of limbal stem cells or limbal tissue can be used to treat LSCD, restoring the corneal surface and improving vision.
Challenges in Transplantation: One of the challenges in limbal stem cell transplantation is rejection and the need for long-term immunosuppression, especially when donor cells are used. Research is ongoing to improve the success rates of these transplants.
Alternative Sources of Stem Cells: Given the limitations in the availability of limbal stem cells, scientists are investigating alternative sources of stem cells, such as induced pluripotent stem cells (iPSCs), which can be reprogrammed to differentiate into corneal epithelial cells.
Gene Therapy: For certain genetic disorders affecting the cornea, gene therapy using corneal stem cells is being explored. This approach involves correcting genetic defects in stem cells and then transplanting them back into the patient’s eye.
Cornea stem cells, particularly limbal stem cells, are a vital area of research and clinical application in ophthalmology. They offer hope for restoring vision in patients with corneal diseases and injuries, and ongoing research continues to expand our understanding and capabilities in using these cells for eye-related therapies.
Stem cells in these organs and tissues play crucial roles in growth, development, and healing. Research into the specific capabilities and uses of these various types of stem cells is ongoing and represents a significant area of interest in regenerative medicine and therapeutic interventions.