Non-small cell lung cancer (NSCLC)
Lung cancer continues to be the leading cause of cancer fatalities. Among its subtypes, Non-small cell lung cancer (NSCLC) occurs most frequently. Treatment options for NSCLC include surgery, radiation, chemotherapy, immunotherapy, and targeted therapy. However, patients undergoing surgery often face the risk of distant metastases or local recurrence. Recent advancements in targeted therapies and immunotherapy have been rapid and significant. Customizing therapy based on individual medical conditions and other factors is essential. Accurate sub-classification of NSCLC, as per the latest World Health Organization guidelines, is crucial for personalized treatment.
Risk Factors
Lung cancer development is linked to several environmental and lifestyle factors. Tobacco smoking accounts for the majority of lung cancer cases, with second-hand smoke, family history, and exposure to carcinogens like radon gas, asbestos, and heavy metals also significantly raising lung cancer risks. Other factors contributing to lung cancer include pulmonary fibrosis, HIV infection, and alcohol consumption.
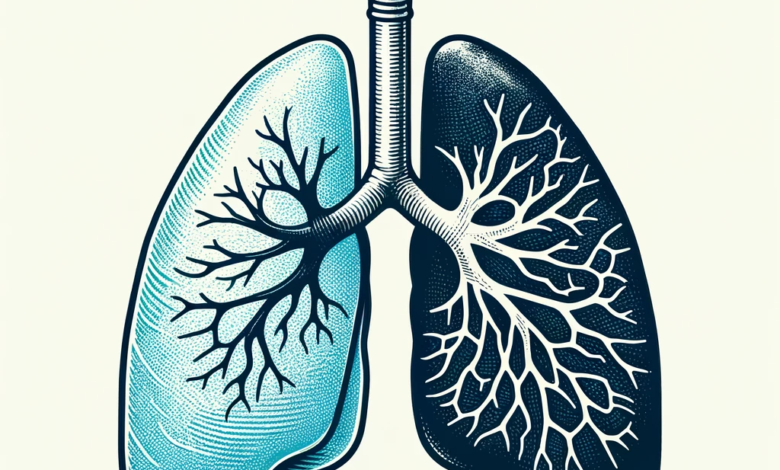
Classification
Lung cancer is primarily categorized into two types: non-small cell lung cancer (NSCLC), which affects 85% of patients, and small cell lung cancer (SCLC), affecting 15%. NSCLC is further divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma, along with various clinical subtypes.
Diagnosis
NSCLC often goes undetected until it reaches an advanced stage. The most common symptom is a cough, experienced by 50 to 75% of patients, along with other symptoms like hemoptysis, dyspepsia, and chest pain.
For more precise staging, positron emission tomography combined with computed tomography (CT) is used to assess lymph node involvement. This approach is supported by findings from another study, which suggest that every lymph node identified as positive on these scans should be examined further.

CT and magnetic resonance imaging (MRI) are commonly used to examine the brain in patients who are receiving treatment aimed at curing the disease or who show signs of brain metastases.
The International Association for the Study of Lung Cancer, along with the American Thoracic Society and the European Respiratory Society, emphasize the importance of obtaining sufficient tissue samples for their new lung cancer classification system. This is crucial for identifying mutations and customizing treatment for all lung tumors initially suspected.
The best method currently available for predicting hemoptysis, a key symptom of lung cancer, is through positive predictive value, which ranges between 2.4–7.5%. The eighth edition of the lung cancer staging system provides a more detailed prognosis for each tumor, node, and metastasis descriptor.
Liquid biopsies are also being employed to identify cancer biomarkers like circulating tumor DNA, microRNA, and circulating tumor cells. In the Noninvasive versus Invasive Lung Evaluation trial involving 282 untreated NSCLC patients, the use of circulating tumor DNA testing offered a less invasive method, enhancing biomarker identification by 48% compared to solely relying on tissue analysis.
Treatment
Treatment for NSCLC involves various methods like surgery, radiation, chemotherapy, immunotherapy, and molecularly targeted therapy. The treatment approach depends on the patient’s overall health and the stage of the disease. For stages I, II, and IIIA NSCLC, particularly when N2 lymph node disease is identified during surgery, curative surgical removal is typically recommended for medically stable patients. Patients in stages II to IIIA are often advised to undergo adjuvant platinum-based chemotherapy post-surgery, despite concerns about high recurrence rates and toxicity. For stage III NSCLC, chemotherapy and immunotherapy are commonly employed. The use of molecularly targeted therapy has been increasing, aiming to enhance survival rates in NSCLC patients, and significant advancements have been made in targeted treatments and immunotherapy.
Surgical Treatment
Surgical intervention aims to excise the tumor and any metastatic lymph nodes from the lung. Achieving a “negative margin,” where no cancer is found in the healthy tissue surrounding the tumor, is crucial. Various surgical procedures are employed in treating NSCLC:
- Lobectomy: Removal of a lung lobe.
- Wedge Resection: Removal of the tumor while preserving as much healthy lung tissue as possible, used when an entire lung lobe cannot be removed.
- Segmentectomy: Similar to wedge resection but often used for larger areas of lung tissues and lymph nodes when a full lung lobe cannot be removed.
- Pneumonectomy: Complete removal of a lung, usually necessary if the tumor is close to the heart. This procedure carries more risk than a lobectomy.
However, there’s a likelihood of distant metastases or local recurrence post-surgery, necessitating adjuvant therapies like radiation, chemotherapy, or targeted therapy. Particularly, patients with Stage IIA, IIB, and IIIA NSCLC often receive chemotherapy post-surgery to eliminate any remaining cancer cells.
Radiation Therapy
In radiation therapy, high-energy beams are utilized to damage the DNA of cancer cells, leading to their destruction. This method can halt or completely eradicate tumors in specific areas of the body. Radiotherapy is particularly beneficial for NSCLC patients who cannot undergo surgery or do not respond to chemotherapy, as it can enhance their life quality as a form of palliative care.

Patients with potentially removable tumors that are not suitable for surgery, or those with Stage I inoperable lung cancer but adequate lung function, might benefit from curative radiotherapy.
For early-stage NSCLC patients with a solitary, small lung nodule and no metastases, stereotactic body radiation therapy is an option. This therapy is not only more cost-effective and convenient for patients but also has been linked to improved survival rates over two years.
Chemotherapy
Chemotherapy employs drugs that target and destroy cancer cells by stopping their growth, division, and spread. It is effective in extending the lifespan and enhancing the quality of life for lung cancer patients at any stage.
Cytotoxic chemotherapy is the primary treatment for Stage IV NSCLC, with its approach tailored according to factors like histology, patient age, coexisting health conditions, and overall health status.
A comprehensive study in France compared the outcomes of surgery with and without preoperative chemotherapy (using mitomycin, ifosfamide, and cisplatin). The study found no overall advantage of adding neoadjuvant chemotherapy, but a detailed analysis showed that preoperative chemotherapy benefits patients with early-stage (N0 and N1) disease, but not those with more advanced (N2) disease.
Reports indicate that chemotherapy, along with epidermal growth factor receptor (EGFR) kinase inhibitors, can improve the median survival rate for patients with advanced-stage cancer, yet the overall survival rate remains relatively low.
Targeted Therapy
Targeted therapy zeroes in on specific genes, proteins, or environmental factors within the tissue that contribute to the growth and survival of tumors. This approach aims to slow down or halt the proliferation and spread of cancer cells without harming healthy cells. The targets vary depending on the type of cancer. To determine the most effective treatment target, patients undergo tests to identify specific genes, proteins, and other elements within their tumors. Some lung cancers exhibit unusually high levels of certain abnormal proteins within the cancer cells. Ongoing research is continually uncovering new details about specific biological targets and innovative treatment approaches.

1- EGFR Inhibitors
In the U.S., a significant percentage of lung cancer patients (10% to 15%) exhibit the EGFR mutation, with a higher incidence (51.4%) in Asian patients. Research has shown that drugs blocking the EGFR pathway can effectively prevent or limit the growth of lung cancer cells harboring this mutation. Several EGFR inhibitors are approved by the FDA, including afatinib, entrectinib, erlotinib, gefitinib, and osimertinib. Recent findings suggest that osimertinib leads to better progression-free survival rates compared to other first-line treatments, thereby becoming the preferred first-line therapy for EGFR-mutant NSCLC.
2-ALK Inhibitors and ROS1 Fusion
The ALK gene plays a role in promoting cancer cell proliferation and is altered in about 5% of NSCLC patients. ROS1 fusions or mutations, though rare, can affect cell development and differentiation and are found in 1 to 2% of NSCLC cases. Drugs targeting ALK and ROS1 mutations include alectinib, brigatinib, ceritinib, lorlatinib, crizotinib, and entrectinib.
3-KRAS G12C Mutation Targeting Drugs
KRAS G12C mutation, a primary genetic alteration in NSCLC patients, occurs in about 20 to 25% of lung cancer cases. Sotorasib is the only drug approved for treating this specific mutation.
4-NTRK Fusion Targeting Drugs
NTRK fusion, a mutation found across various tumor types, can drive cancer cell growth. It is, however, less common in lung cancer patients (<1%). Larotrectinib, an oral inhibitor, is approved for treating advanced cancers with NTRK fusion in patients lacking alternative treatment options.
5-BRAF V600E Mutation Targeting Drugs
Around 2% of NSCLC patients have BRAF mutations, with BRAF V600 mutations comprising half of these cases. Vemurafenib has shown promising results, and the FDA has approved dabrafenib and trametinib for patients with this mutation who have not responded to chemotherapy.
6- MET Exon 14 Skipping Targeting Drugs
Disruptions in the MET proto-oncogene lead to MET exon 14 skipping, affecting tumor growth and spread, and are present in about 3 to 4% of NSCLC cases. Approved treatments for this mutation include capmatinib and tepotinib.
7-RET Fusion Targeting Drugs
A small percentage of NSCLC patients (up to 2%) exhibit RET fusion. Pralsetinib and selpercatinib have been authorized for treating patients with this condition.
8-Vascular Endothelial Growth Factor Targeting Drugs
Angiogenesis therapies focus on inhibiting blood vessel formation, essential for tumor growth and spread. Anti-angiogenesis medications, such as bevacizumab combined with chemotherapy and other drugs targeting vascular endothelial growth factors, are used to ‘starve’ the tumor of necessary nutrients.
Immunotherapy
Immunotherapy, also known as biological therapy, is employed to bolster the body’s innate cancer-fighting mechanisms. It involves the use of natural or man-made substances to improve, direct, or rejuvenate the functions of the immune system. Modern cancer treatment advancements are focused on creating drugs that influence the immune system’s interaction with cancer cells. Immunotherapy is effective regardless of the mutation status in cancer cells and typically has fewer side effects. Clinical research has shown the efficacy of treatments targeting PD-1, CTLA4, and PD-L1.

For NSCLC patients, immunotherapy options include single-agent immunotherapy, combinations of different immunotherapy drugs, or a mix of immunotherapy and chemotherapy. These approaches are especially useful for treating advanced NSCLC resistant to other targeted therapies.
Studies like CheckMate 017 and 057 have demonstrated the significant anti-cancer effectiveness of the PD-1 inhibitor nivolumab in extensively treated metastatic cases. Updated survival analyses reveal that nivolumab offers a substantial survival advantage over docetaxel, leading to a significant increase in overall survival rates. Consequently, the FDA has approved nivolumab for treating metastatic NSCLC.
PD-1 Pathway Blockers
The PD-1 pathway plays a vital role in the immune system’s ability to suppress tumor growth. Medications that inhibit PD-1 and PD-L1 have been effective in slowing or stopping the progression of NSCLC. The FDA has approved three such drugs for NSCLC: atezolizumab, nivolumab, and pembrolizumab. Nivolumab is commonly used as a second-line treatment for metastatic NSCLC patients, particularly those who have not responded to platinum-based chemotherapy, as it offers improved survival rates with lower toxicity.
Pembrolizumab received expedited FDA approval for use in NSCLC patients with high PD-L1 expression in advanced or inoperable tumors.
CTLA-4 Pathway Blockers
Targeting the CTLA-4 pathway is another approach in immunotherapy. The FDA has approved ipilimumab, an inhibitor of NSCLC progression, for use in combination with nivolumab as part of a chemotherapy regimen. This treatment typically has fewer severe side effects than conventional chemotherapy, though immunotherapy can cause various side effects, including skin reactions, flu-like symptoms, shortness of breath, and weight changes.
Conclusion
reatment plans for NSCLC patients vary according to the stage of the disease, necessitating personalized therapy that takes into account each individual’s unique medical condition and other factors.
The integration of immunotherapy with targeted therapy represents a significant advancement in NSCLC treatment. Immunotherapy, whether used alone or combined with chemotherapy, has established itself as the primary initial treatment approach.
Despite significant advancements in targeted therapy and immunotherapy, the overall progression-free survival (PFS) rate for lung cancer patients continues to be unsatisfactory. Adhering to the latest WHO guidelines, precise sub-classification of NSCLC is essential for devising customized treatment strategies.