Strep A outbreaks

It is generally rare for group A beta-hemolytic streptococcus bacteria to cause an invasive disease. There has been a significant increase in cases reported since 2022, especially in some countries. There has been an increase in the UK and Ireland in the European region since September. Other European countries have also reported cases, including France, the Netherlands, Germany, and others. In Australia and New Zealand, there have been an increase in case reports. As a general rule, invasive strep A infections progress a lot more rapidly when they cause high mortality, especially in the United Kingdom and the Netherlands, where case losses have been reported.
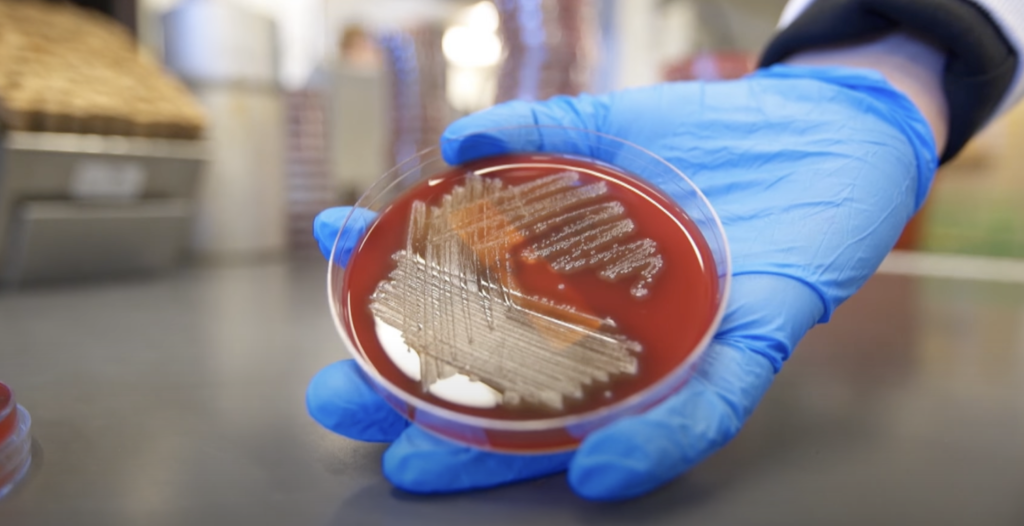
There are more than 500,000 deaths worldwide every year caused by Streptococcus pyogenes, a Gram-positive bacterium often found in the throat and skin.
In school-aged children, streptococcal tonsillitis is considered a common cause of tonsillopharyngitis. The infection can also lead to streptococcosis in younger children. Winter and early spring are the peak seasons for strep A pharyngitis. Kindergartners and primary school students are most likely to experience outbreaks.
Impetigo is the most common skin infection seen during the summer, however erysipelas and cellulitis are also common. There are some strains of strep A that secrete pyrogenic exotoxins (erythrogenic toxin). Scarlet fever occurs when these exotoxins are encountered for the first time, causing rash and fever. Strep A tonsillopharyngitis and skin infections may occur more than once because there are numerous strains of the bacteria. Because of the antibodies developed against exotoxins, scarlet fever usually only occurs once.
There are also cases of Strep A causing invasive infections that can be life-threatening. During invasive Strep A infection, bacteria are isolated from normally sterile body areas like the blood, joints, or lungs. A person who is infected can transmit the disease through droplets (cough, sneeze), close contact, or direct contact with a wound.
Acute tonsillopharyngitis
In children, high fevers, sore throats, difficulty swallowing; absence of cough, runny noses, stuffy noses, tearing or redness; on physical examination, hyperemia (may or may not be exudate) and tender lymphadenopathy in the tonsils and pharynx indicate Strep A tonsillopharyngitis.
In adults, CENTOR criteria can also be used to diagnose tonsillopharyngitis caused by strep A.
CENTOR criteria:
1-Fewer
2-Exudate on the tonsils,
3-Coughs and colds (runny noses) are not present,
4-There is tenderness in the anterior cervical lymph nodes
It is important to note that the presence of 3 or 4 findings in patients is indicative of the diagnosis of GAS tonsillopharyngitis, especially in studies conducted with adults.
